 Oct, 11 2025
Oct, 11 2025
Private Healthcare Cost Calculator
Calculate Your Private Healthcare Costs
See how private healthcare compares financially to NHS services
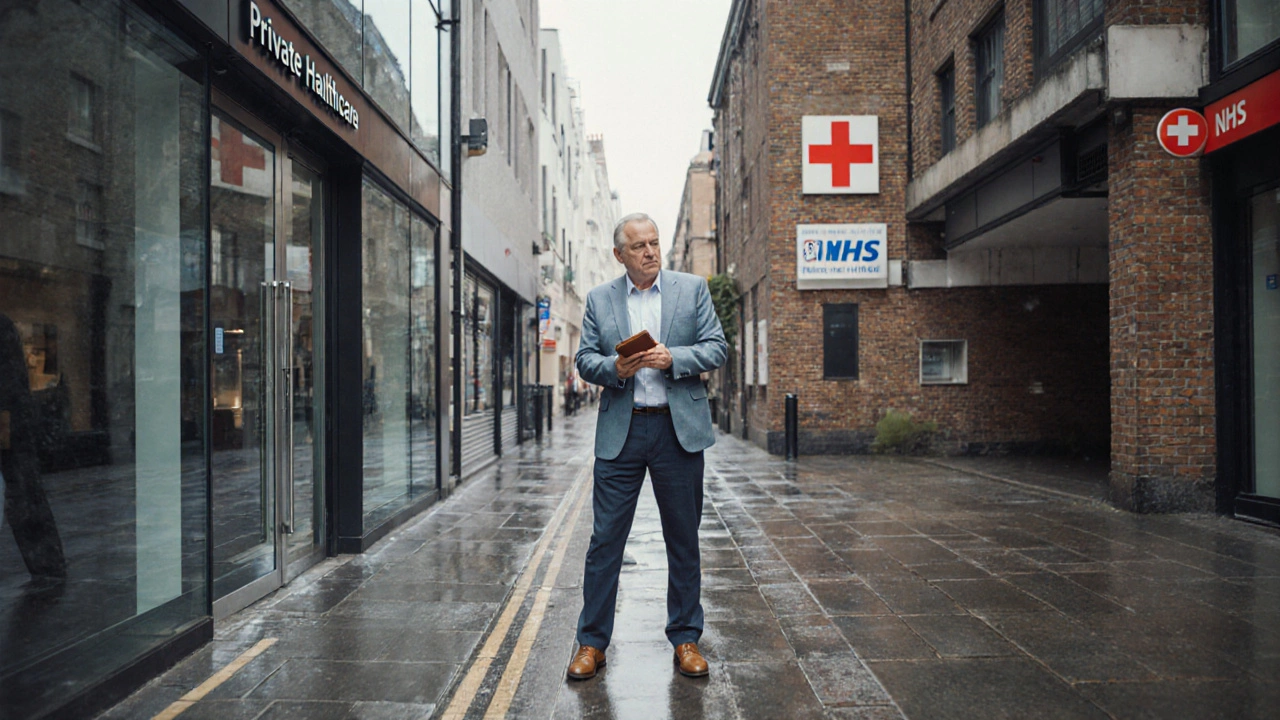
When people hear "private healthcare" they picture fast appointments, fancy facilities, and personalized treatment. The reality in the UK, however, is a mixed bag. While private options can fill gaps left by the NHS, they also bring a set of drawbacks that affect cost, fairness, and even the quality of care you receive.
Key Takeaways
- Private care often costs far more than NHS services and can lead to unexpected out‑of‑pocket bills.
- It can widen health inequality because only those who can afford it get timely access.
- Profit‑driven models sometimes compromise continuity of care and patient safety.
- Regulation is less stringent than the NHS, making complaints harder to resolve.
- Choosing private care may not guarantee better outcomes for routine conditions.
Private Healthcare is a sector where patients pay directly or through private insurers for medical services that are also offered by the public system. In the UK it sits alongside the National Health Service (NHS), which provides free‑at‑point‑of‑use care funded by taxes. Understanding the downsides helps you decide whether private routes are worth the extra cash.
1. High Out‑of‑Pocket Costs
The most obvious downside is the price tag. A typical private consultation can run from £150 to £300, and surgical procedures often cost several thousand pounds even after insurance. When you add diagnostic tests, medication, and follow‑up visits, the total can quickly exceed what the NHS would have covered for free.
Insurance policies may lower the bill, but they come with premiums, excesses, and strict coverage limits. A 2023 survey of UK private insurers showed the average annual premium for an individual was £1,200, with many policies excluding pre‑existing conditions.
2. Widening Health Inequality
Because private services rely on ability to pay, they tend to favor affluent groups. This creates a two‑tier system: wealthier patients enjoy quicker appointments, while lower‑income individuals remain stuck on NHS waiting lists. A 2022 Health Foundation report found that people in the top 10% of earners were twice as likely to use private hospital care compared with the bottom 10%.
Consequences extend beyond individual health. When a sizable portion of the population opts out of the NHS for private care, public resources can become strained, potentially lengthening waiting times for those who rely solely on the NHS.
3. Variable Quality and Continuity of Care
Private clinics often advertise state‑of‑the‑art facilities, but quality isn’t guaranteed across the board. Some providers prioritize high‑volume, low‑cost procedures that may compromise thoroughness. Continuity suffers when a patient sees a different specialist at each visit because the clinic contracts with multiple freelancers.
Contrast this with the NHS, where most patients have a named GP who coordinates referrals and maintains a comprehensive record. Private patients can end up with fragmented records, especially if they switch providers or rely on multiple insurers.
4. Less Stringent Regulation and Redress
While the Care Quality Commission (CQC) inspects both NHS and private facilities, private providers sometimes operate under slightly looser oversight, especially for boutique clinics that focus on cosmetic or elective procedures. This can make it harder to lodge complaints or obtain compensation when things go wrong.
In addition, the legal route for malpractice claims in private practice can be more complex, involving private insurers who may seek to settle for lower amounts to protect their own bottom line.
5. Impact on Waiting Times
One argument for private care is that it relieves pressure on the NHS, shortening waiting times for everyone. In practice the effect is modest. A 2024 analysis of NHS waiting list data showed only a 3% reduction in elective surgery backlogs in regions with higher private sector usage.
Meanwhile, private patients often face their own scheduling delays when demand spikes, especially for popular procedures like orthopaedic surgery or IVF, where private clinics can be fully booked weeks in advance.
6. Profit Motive Can Skew Priorities
Private providers need to turn a profit. This can steer them toward services with higher margins, such as cosmetic surgery or diagnostic imaging, rather than focusing on essential but less lucrative care like chronic disease management.
When profit drives decision‑making, patients may be nudged toward unnecessary tests or treatments that boost the clinic’s revenue, a practice known as “over‑diagnosis.”
7. Limited Coverage for Chronic and Complex Conditions
Private insurance often caps the number of covered sessions for physiotherapy, mental health counseling, or long‑term disease monitoring. Patients with chronic illnesses may find themselves paying out‑of‑pocket for ongoing care that the NHS would provide at no cost.
For example, a private health plan might allow only ten physiotherapy sessions per year, whereas a chronic back‑pain sufferer could need monthly sessions for several years.
Comparison at a Glance
| Aspect | Private Healthcare | NHS |
|---|---|---|
| Cost to Patient | High direct fees or insurance premiums | Free at point of use |
| Waiting Times | Generally shorter for elective services, but variable | Longer for elective surgeries, improving slowly |
| Continuity of Care | Often fragmented across providers | Coordinated through GP and integrated records |
| Regulation | Subject to CQC, but oversight can be lighter | Strict national standards and public accountability |
| Equity | Access tied to ability to pay | Universal access regardless of income |
| Scope of Services | Focus on profitable, elective procedures | Broad range including chronic disease management |
8. Practical Tips If You Still Want Private Care
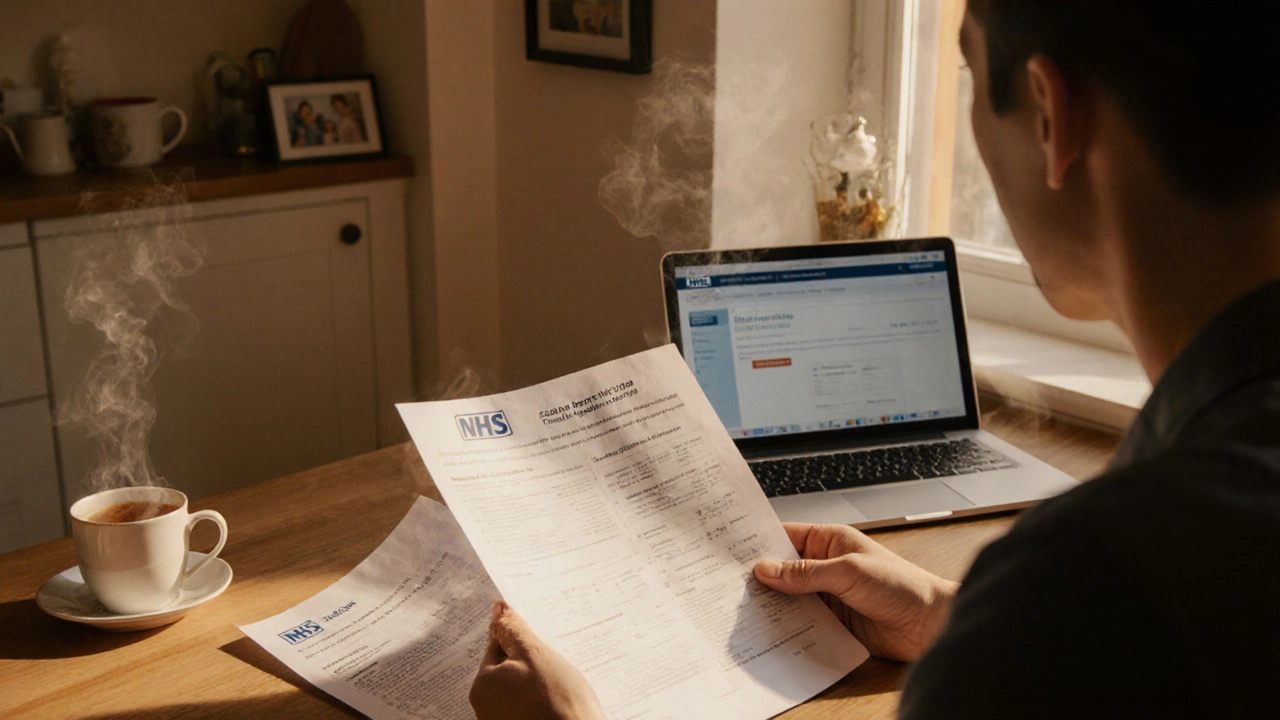
- Check your insurance policy carefully - note exclusions, caps, and the required pre‑authorisation process.
- Ask for a detailed cost estimate before any procedure. Verify if follow‑up visits are included.
- Research the provider’s CQC rating and look for patient reviews that mention safety and after‑care.
- Consider using private care only for services with proven speed or quality benefits, such as certain imaging tests or specialist consultations that the NHS cannot provide promptly.
- Maintain a copy of all medical records and share them with your NHS GP to avoid duplication and ensure continuity.
Private healthcare can be a useful supplement, but the disadvantages listed above mean it isn’t a one‑size‑fits‑all solution. Weigh the financial hit against the real benefits you expect.
Frequently Asked Questions
Is private healthcare always faster than the NHS?
Speed varies. Private clinics can often schedule elective procedures within weeks, but high demand for popular surgeries can still cause delays. The NHS may have longer waits for elective work, yet urgent or emergency care is uniformly fast.
Do private health insurers cover all medical costs?
No. Most policies have limits on certain treatments, exclusions for pre‑existing conditions, and require co‑payments. Always read the fine print and ask for a coverage summary.
Can private care affect my NHS eligibility?
Using private services does not strip you of NHS rights. You can still register with a GP and access NHS care whenever you need it.
What should I look for in a private clinic’s CQC rating?
Aim for "Outstanding" or "Good" ratings. Check inspection reports for safety incidents, staffing levels, and patient feedback on continuity of care.
Are there any tax advantages to using private healthcare?
Employers can provide private health insurance as a benefit, and the cost is often treated as a taxable benefit in kind. For individuals, premiums are generally not tax‑deductible.
