 Jun, 29 2025
Jun, 29 2025
You ever leave a doctor’s office and wonder, Did I just say something dumb? Imagine that tension multiplied if you’re at a pain clinic and the stakes are higher than usual. Some folks think pain management doctors are just pill dispensers; others worry their honest answers will be used against them. Guess what? Both are wrong. These doctors are people, but their world comes with paperwork, red flags, and the constant pressure to separate legit patients from those just chasing prescriptions. Saying the wrong thing, even by accident, can lead you down a path you never wanted to walk, like being dismissed or flagged in your records. Some things are better left unsaid—or at least said in a seriously thoughtful way.
Why Your Words Matter in a Pain Clinic
Pain doctors don’t have crystal balls. They have their experience, your medical file, and what you tell them. If your words sound rehearsed or desperate, red lights flash. A classic trap is sounding like you googled "how to get pain meds," which is a big no-go. These doctors get training about drug-seeking behavior, so anything that looks off sticks in their mind. Did you know a January 2022 survey of pain management doctors found that 74% have denied patients meds based on suspicious conversations, not just test results? If you mention certain phrases—like asking for a specific drug by name, or saying nothing else works except one powerful opioid—it can spark a deep dive into your medical history. These visits go into your permanent health records, so being careful is smart. This doesn’t mean you need to hide your pain, but style and honesty matter. Little details—like exaggerating symptoms, demanding immediate medication, or acting frustrated when doctors suggest non-opioid options—raise eyebrows. If you’re in this to get real help, don’t give them a reason to mistrust you.
What Not to Say: Examples That Can Backfire
Let’s break down the biggest "oops" moments. First up: “I lost my pills again.” Sure, it happens. But say it twice and you’re seen as careless or worse, a potential abuser. Then there’s “That dose doesn’t do anything for me” and “Only Oxy works for my pain.” If it sounds like you’re shopping for a fix, they might start thinking you’re not serious about getting to the root of your pain. Sometimes people even quote data wrong, like, “I read that strong opiates are the only thing that works for nerve pain”—not true. Doctors know their studies. Try to avoid talking only about pain scores (“Today it’s 10 out of 10, yesterday it was 4, now it’s 8, sometimes it’s negative 2”), because wildly changing numbers make it hard for your doctor to get a real picture. Another red flag: “Whatever you gave me last time barely touched my pain.” It sounds like you’re requesting something stronger every visit. And if you ever say, “I know someone who gets more than me,” stop. Your care isn’t a contest. One more: “I ran out early.” Doctors know how long a prescription should last, and this is a huge warning sign for them. If it happens once, explain clearly. But make it a habit, and you’ll probably lose trust—fast.

The Science of Honest Pain Communication
So how do doctors actually figure out if someone’s pain is real? Truth is, chronic pain doesn’t usually show up in blood tests or x-rays. A 2023 study in the Journal of Pain Research found less than 40% of chronic pain cases have clear imaging proof. That means pain management doctors rely on your story, daily impact, how symptoms shift, and how you respond to various treatments. They look for consistency. You don’t need to act tough or dramatic—just stick to facts: what hurts, when, what makes it better or worse, and how it gets in the way of your life. The best patients are honest about their limits (“Walking from my door to my mailbox hurts most days, but I can manage groceries with breaks”). Specific details help: “Sharp, burning pain when I sit, but throbbing when I stand.” If you’re nervous, write notes before the appointment. Track your symptoms using a pain diary. The honesty you bring helps doctors spot patterns, link pain to possible causes, and figure out which treatments might help. Remember, they have access to state prescription monitoring programs—so hiding ER visits or extra scripts always backfires. Trust is a two-way street.
Common Traps: What Well-Meaning Patients Get Wrong
Even if you aren’t drug-seeking, it’s easy to slip up. You want relief. You want to be understood. But some phrases just don’t help your case. Here are a few common traps:
- Oversharing emotional distress. Yes, pain makes you anxious or depressed. But if you lead with “I’m so anxious, nothing helps, I can’t live like this,” a doctor may think you need a mental health referral instead of pain treatment.
- Fixating on old methods. Saying, “Only injections work—don’t bother with anything else,” closes the door to better, safer treatments.
- Withholding substance use. If you drink, smoke weed, or take someone else’s pills, hiding it may land you in dangerous territory with drug interactions.
- Jumping from doctor to doctor. If you tell your pain doc your last few doctors “just wouldn’t help” or “didn’t get it,” you look like you’re shopping for a new prescription—not help.
- Ignoring non-medication options. Dismissing suggestions like physical therapy or counseling tells doctors you only want pills, not a real solution.
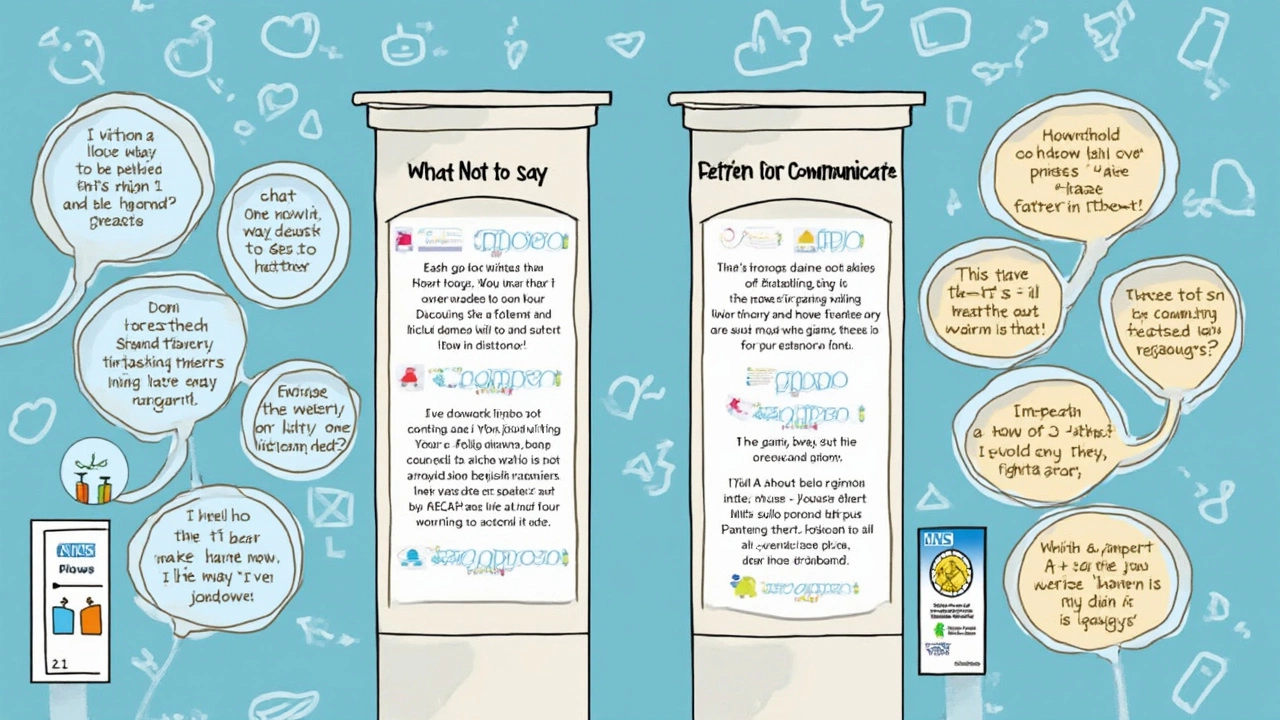
How to Have Productive, Honest Conversations With Your Doctor
The best approach? Be direct, but thoughtful. Say, “Here’s what I’m feeling, here’s how it changes my day, here’s what I’ve tried.” If you tried medication or therapy and it failed, mention how it failed—side effects, no relief, or got worse. Avoid saying nothing works, period. Instead, say, “I didn’t notice much improvement, but I’m open to trying what you think makes sense.” This shows you’re not fixated on one outcome. Share your goals—maybe you just want to walk your dog without agony, or get through a work shift without wincing. When you speak about medication, frame it as one tool in your box, not something you’re demanding. If you misuse a medication (ran out early, lost a script), admit it upfront, explain what happened, and ask for strategies to prevent it happening again. This honesty actually builds trust.
Your doctor doesn’t expect you to be a pain scholar. They do expect you to be honest, engaged, and willing to work together. That means some weeks are harder than others; some attempts will flop, and sometimes you’ll leave disappointed. But if you keep communication honest, consistent, and focused on real improvement instead of just prescriptions, your odds of building a lasting, trusting relationship go way up. You want your doctor to see you as a person, not a problem. Let your words help you get there.
