 Jan, 4 2026
Jan, 4 2026
Chronic Pain Tracker
Track Your Pain Today
Log your pain intensity, triggers, and interventions to identify patterns. Based on evidence from The Lancet and University of Auckland studies.
Your Pain Insights
Track patterns to identify what works best for you. Evidence shows exercise reduces pain by 30-50% and CBT improves quality of life.
Chronic pain doesn’t go away after an injury heals. It lingers for months or years, turning everyday movements into battles. People with chronic pain aren’t just looking for comfort-they’re searching for a way to live again. The question isn’t just what’s the strongest pain relief, but what actually works without wrecking your life.
There’s no single ‘strongest’ solution
Many assume the strongest pain relief means the strongest drug. That’s a dangerous myth. Opioids like oxycodone or fentanyl might numb the sensation, but they don’t fix the problem. And over time, they make pain worse. A 2023 study from the University of Auckland tracked 1,200 people with chronic back pain over five years. Those on long-term opioids reported higher pain levels and more disability than those who used non-drug methods.
Chronic pain isn’t just a signal-it’s a rewiring of your nervous system. Your brain starts interpreting normal sensations as threats. That’s why the best treatments don’t just block pain signals. They retrain your body’s response.
What actually works: evidence-backed options
Here’s what real research shows works for long-term pain control:
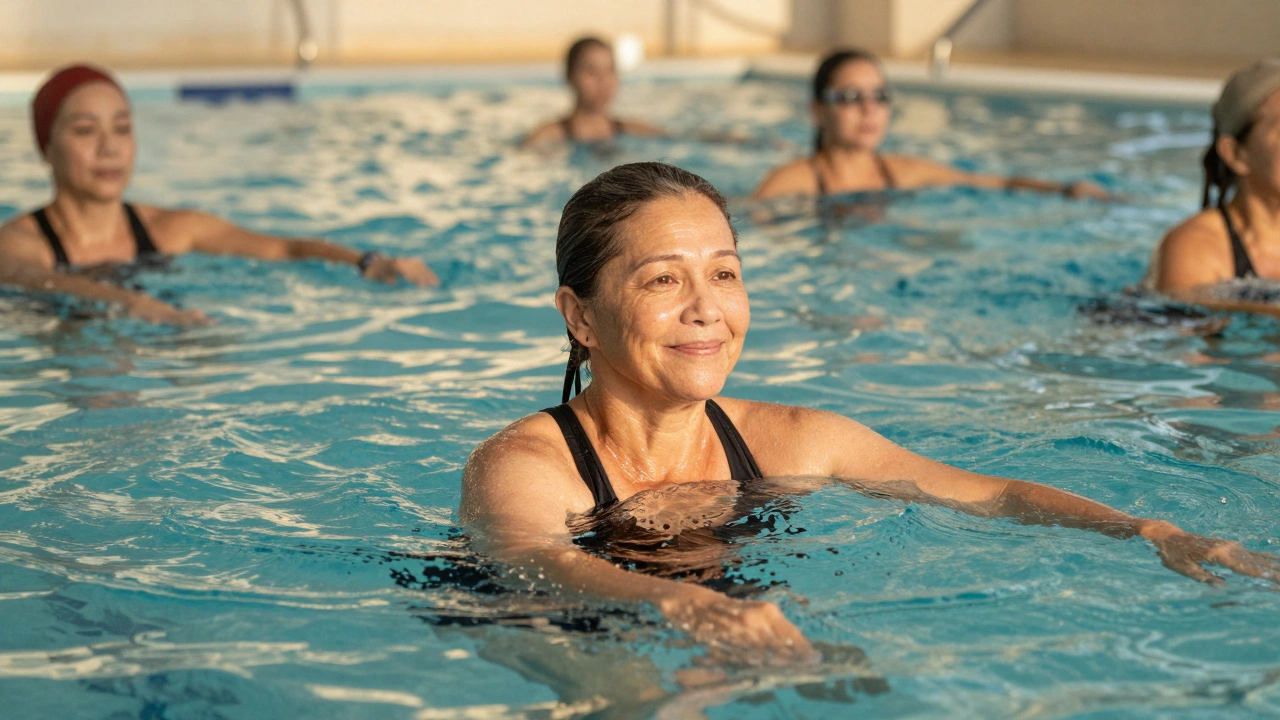
- Exercise therapy - Not just walking. Structured programs like aquatic therapy, tai chi, or graded movement therapy reduce pain intensity by 30-50% in 8-12 weeks. A 2024 meta-analysis in The Lancet found exercise was more effective than most painkillers for osteoarthritis and fibromyalgia.
- Cognitive Behavioral Therapy (CBT) - CBT doesn’t pretend pain isn’t real. It teaches you how to stop letting pain control your thoughts. People who complete 10-12 sessions report better sleep, less anxiety, and reduced pain interference in daily life.
- Neuromodulation - Devices like spinal cord stimulators or peripheral nerve stimulators send mild electrical pulses to interrupt pain signals. For people who’ve tried everything else, these can cut pain by 50% or more. The success rate is highest for complex regional pain syndrome and failed back surgery syndrome.
- Topical treatments - Lidocaine patches, capsaicin creams, and compounded gels with ketamine or gabapentin applied directly to the skin avoid systemic side effects. They’re especially helpful for localized nerve pain like postherpetic neuralgia.
- Multidisciplinary pain clinics - These aren’t just doctors. They’re teams: physiotherapists, psychologists, occupational therapists, and pain specialists working together. Patients in these programs are 40% more likely to return to work and 60% less likely to need surgery.
Medications: use them smartly, not as crutches
Some drugs still have a place-but only when used carefully and short-term.
- Gabapentin and pregabalin - These work for nerve pain. They’re not opioids, but they can cause dizziness, weight gain, and brain fog. Use them only if you have confirmed nerve damage (like diabetic neuropathy).
- Antidepressants (SNRIs like duloxetine) - These aren’t for depression. They help regulate pain signals in the brain. Studies show they reduce chronic pain by 30% on average. Side effects? Dry mouth, nausea, sleep changes. Worth it for many.
- NSAIDs (ibuprofen, naproxen) - Fine for occasional flare-ups, but dangerous long-term. They raise blood pressure, damage kidneys, and cause stomach ulcers. Don’t use daily for more than 10-14 days without medical supervision.
- Opioids - Avoid unless under strict supervision for severe, short-term pain after surgery or cancer. For non-cancer chronic pain, they’re not recommended by any major medical body in the U.S., UK, Australia, or New Zealand. The risks-addiction, overdose, tolerance, worsening pain-far outweigh any short-term benefit.

The hidden factor: inflammation and lifestyle
Chronic pain often flares with inflammation. And inflammation doesn’t come from just injury. It comes from sleep loss, stress, processed food, and sitting too long.
One patient I worked with in Auckland had severe lower back pain for seven years. She tried injections, physical therapy, even acupuncture. Nothing stuck. Then she changed three things: she cut out sugary drinks, started walking 20 minutes a day, and got 7 hours of sleep instead of 5. Within six weeks, her pain dropped from an 8/10 to a 3/10. No new meds. No surgery.
Anti-inflammatory diets-rich in omega-3s (salmon, flaxseed), leafy greens, berries, and nuts-can reduce pain markers in the blood. Sleep is non-negotiable. Poor sleep increases pain sensitivity by up to 40%. Stress management? It’s not optional. Cortisol, the stress hormone, directly amplifies pain signals.
What doesn’t work-and why you should avoid it
There’s a booming industry selling false hope:
- Herbal ‘miracle’ supplements - Turmeric, CBD oil, devil’s claw. Some show mild effects in small studies, but most lack standardization. You don’t know how much active ingredient you’re getting. And CBD can interact with blood thinners and antidepressants.
- Long-term steroid injections - These can weaken tendons and cartilage. Repeated use in joints like knees or shoulders can cause permanent damage.
- Chiropractic adjustments for non-mechanical pain - If your pain isn’t from a pinched nerve or joint misalignment, spinal cracking won’t help. It might even make it worse.
- Buying painkillers online - Fake pills with fentanyl or carfentanil are flooding the dark web. In New Zealand, overdose deaths from counterfeit drugs rose 22% in 2024. Never buy meds without a prescription from a licensed provider.

When to see a specialist
See a pain specialist if:
- Your pain hasn’t improved after 6-8 weeks of basic treatment (exercise, heat, rest)
- You’re taking more than 75 mg of morphine equivalent per day
- You’re avoiding social activities, work, or family because of pain
- You’ve tried at least two different types of non-drug treatments without success
Specialists don’t just hand out prescriptions. They map your pain: what triggers it, what calms it, how it affects your mood and movement. Then they build a plan-no cookie-cutter solutions.
Real-life example: Sarah’s journey
Sarah, 52, had fibromyalgia for 12 years. She took 400 mg of gabapentin daily, plus oxycodone for flare-ups. She couldn’t walk her dog, cook dinner, or play with her grandkids. Her doctor referred her to a multidisciplinary pain clinic.
She dropped opioids. Started CBT. Did water aerobics three times a week. Added magnesium and vitamin D. Cut caffeine. Within four months, she stopped all opioids. Her pain dropped from 9/10 to 4/10. She started gardening again. She slept through the night.
She didn’t find the strongest pain relief. She found the right relief-for her.
Your next steps
Start here:
- Track your pain for a week. Note intensity (1-10), triggers (stress, weather, activity), and what helps (heat, rest, movement).
- See your GP. Ask for a referral to a pain specialist or multidisciplinary clinic.
- Start moving-even 10 minutes of walking daily. Movement is medicine.
- Eliminate one thing that worsens inflammation: sugary drinks, processed snacks, or late-night screen time.
- Ask about CBT. It’s covered by most private health plans in New Zealand.
Chronic pain is not a life sentence. But it’s not a quick fix either. The strongest relief isn’t found in a pill bottle. It’s built-day by day, choice by choice-with movement, mindset, and medical support.
What is the strongest pain relief for chronic pain?
There’s no single strongest pain relief for chronic pain. Strong opioids may seem powerful, but they often make pain worse over time. The most effective approach combines physical therapy, cognitive behavioral therapy, nerve-targeted treatments like spinal stimulation, and lifestyle changes. Evidence shows these methods reduce pain intensity by 30-50% long-term without the risks of addiction or tolerance.
Are opioids the best option for chronic pain?
No. Major health organizations-including the CDC, WHO, and New Zealand’s Ministry of Health-no longer recommend opioids for long-term chronic pain. They increase the risk of addiction, overdose, and even heighten pain sensitivity over time (a condition called opioid-induced hyperalgesia). For non-cancer chronic pain, the risks far outweigh any short-term benefit.
Can exercise really help with chronic pain?
Yes. Studies show structured movement-like water therapy, tai chi, or graded exercise-reduces chronic pain by 30-50% in 8-12 weeks. Exercise doesn’t just strengthen muscles. It lowers inflammation, releases natural painkillers (endorphins), and retrains the nervous system to stop overreacting to pain signals. Start slow. Consistency matters more than intensity.
What’s better than painkillers for chronic pain?
Non-drug treatments like cognitive behavioral therapy (CBT), spinal cord stimulation, physical therapy, and anti-inflammatory lifestyle changes are more effective long-term than painkillers. CBT helps rewire how your brain processes pain. Movement rebuilds function. Sleep and diet reduce inflammation. These work together to restore quality of life without dangerous side effects.
Is CBD oil good for chronic pain?
Some people find mild relief, but evidence is limited and inconsistent. CBD products are poorly regulated-you don’t know how much actual CBD is in them. They can also interact with medications like blood thinners or antidepressants. Don’t rely on CBD as a primary treatment. Use it only as a supplement, and only after talking to your doctor.
How do I know if I need a pain specialist?
See a pain specialist if your pain lasts more than 3 months, doesn’t improve with basic treatments, or is affecting your sleep, work, or relationships. Specialists don’t just prescribe drugs-they create personalized plans combining physical, psychological, and medical approaches. Most private health insurers in New Zealand cover these services.
