 Nov, 17 2025
Nov, 17 2025
Free healthcare sounds like a dream-no bills at the hospital, no panic when your kid gets sick, no choosing between medicine and groceries. But if you’ve ever waited six months for a knee scan or watched someone skip a follow-up because the waitlist was too long, you know free doesn’t always mean fast or easy. In countries like New Zealand, the UK, and Canada, public healthcare systems are funded by taxes and offered to everyone. But behind the promise of universal access are real trade-offs that affect how care actually works on the ground.
Long Wait Times Are the Biggest Complaint
One of the most common complaints about free healthcare isn’t that it’s expensive-it’s that it’s slow. In New Zealand, the public system routinely sees waits of 12 to 18 weeks for non-urgent surgeries like hip replacements. In the UK’s NHS, over 7 million people were on waiting lists in early 2025, with some waiting over a year for specialist consultations. These aren’t outliers. They’re the norm.
Why? Because resources are limited, and demand is endless. When everyone gets the same access regardless of income, the system gets flooded. A broken wrist might get seen in a day. But a chronic back pain issue? You might wait months. And if you’re in pain now, waiting isn’t just inconvenient-it’s debilitating.
Doctors Are Overworked and Underpaid
Public healthcare systems rely on doctors who are often stretched thin. In New Zealand, general practitioners (GPs) are paid a flat fee per patient, not per service. That means they can’t afford to spend extra time with each person without losing money. Many GPs now see 40+ patients a day, with 7-minute appointments the standard.
As a result, burnout is high. Nearly 40% of public hospital doctors in Australia and New Zealand reported considering leaving the profession in 2024, according to a joint medical association survey. When staff are exhausted, mistakes happen. Missed diagnoses, rushed consultations, and delayed referrals become more common-not because doctors are careless, but because they’re running on empty.
Lower Quality of Equipment and Facilities
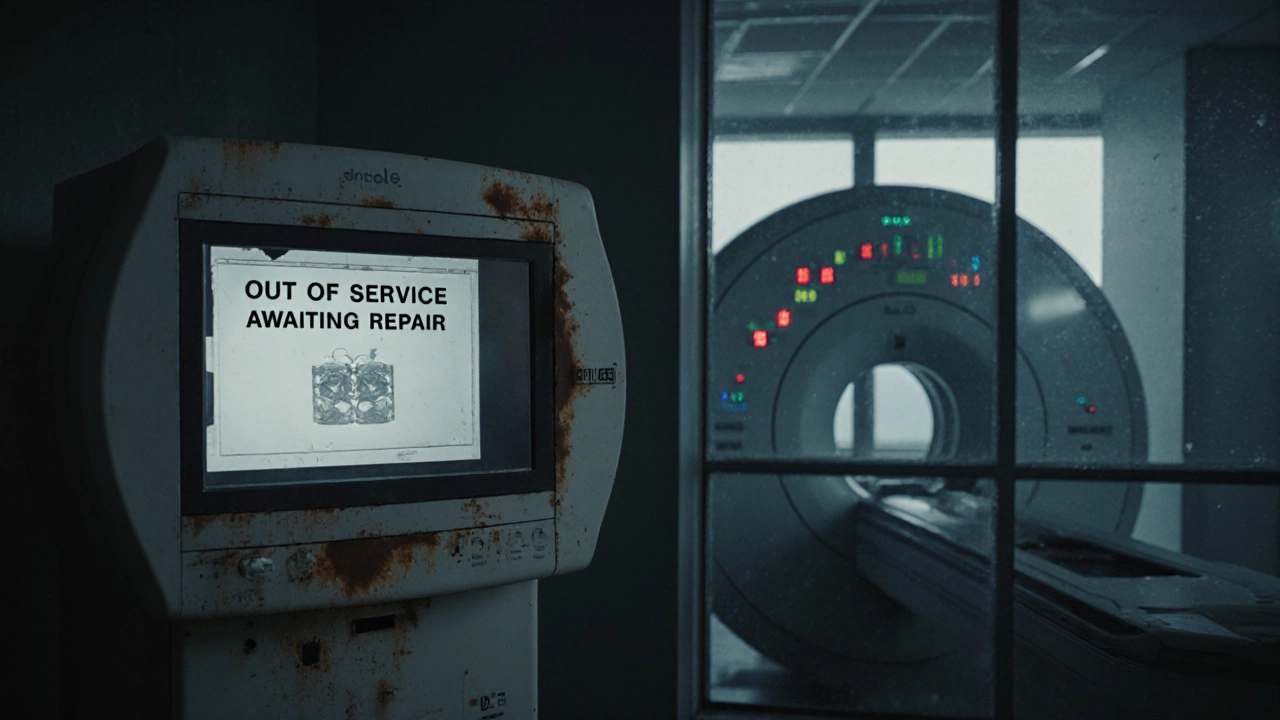
Public hospitals often use older equipment and outdated infrastructure. A 2024 audit of New Zealand’s public hospitals found that 32% of MRI machines were over 12 years old, well past their recommended lifespan. Some rural clinics still use film-based X-rays because digital upgrades haven’t been funded.
Compare that to private clinics, where new machines are installed every 5-7 years. Modern imaging tools catch early signs of disease that older tech misses. In a public system, you might get a diagnosis six months later-or not at all-because the machine broke down and the repair budget was cut.

Less Choice in Providers and Treatments
With free healthcare, you don’t get to pick your surgeon, your hospital, or even your doctor. You’re assigned based on availability. If you want a specific specialist who’s known for better outcomes, you can’t just book them-you have to wait for them to be assigned to you, if they’re even in the system.
Some treatments are simply not covered. Cosmetic procedures are obvious, but even some physical therapies, mental health programs, and alternative pain treatments are excluded. For example, acupuncture for chronic back pain might be available privately, but not through public funding. If you want it, you pay out of pocket-or go without.
Hidden Costs and Hidden Inequities
Free healthcare isn’t free-it’s paid for with taxes. In New Zealand, the average household pays over $8,000 a year in taxes that fund public health. That’s money taken from families who may never use the system, or use it only minimally.
And here’s the twist: the people who benefit most from public healthcare are often those who can’t afford private care. But the people who pay the most are middle-income earners who could easily afford a private plan. Meanwhile, high-income earners might pay more in taxes but still use private services for faster access, creating a two-tier system in disguise.
Drug and Medicine Shortages
Public systems negotiate bulk drug prices to keep costs low. But that means they often choose the cheapest option, not the best one. If a new cancer drug costs $10,000 a dose and a generic version works 85% as well, the public system will go with the generic-even if the patient might respond better to the new one.
Medication shortages are also more common. In 2023, New Zealand’s public health system ran out of insulin for over 3,000 patients for nearly two weeks. No one died, but many had to ration doses or switch to less effective alternatives. Private patients rarely face this-they can pay extra to get the right drug, right away.
Delayed Innovation and Slower Adoption of New Tech
When funding is tight and bureaucracy is slow, new medical tech takes years to roll out. Robotic surgery, AI-assisted diagnostics, and telehealth platforms are adopted faster in private clinics. In public hospitals, approval for new tech can take 2-4 years just to get through funding committees.
For example, AI tools that can detect early signs of diabetic retinopathy from a simple eye scan are already being used in private practices across Auckland. But in public hospitals, they’re still being tested in pilot programs. That means patients in the public system miss out on early detection-and the chance to prevent blindness.
It’s Not About Being ‘Unfair’-It’s About Trade-Offs
People often argue that free healthcare is a moral good. And it is-for those who can’t pay. But the system doesn’t work by magic. Every dollar spent on one thing is a dollar not spent on another. More nurses? Fewer scanners. Faster access? Higher taxes. Better drugs? Fewer treatment options.
Free healthcare doesn’t mean better care. It means equal access to limited care. And when demand outstrips supply, someone always waits. Sometimes, that someone is you.
What Can You Do If You’re Affected?
If you’re stuck in long waits or denied treatments, here are a few practical steps:
- Keep detailed records of symptoms, dates, and communications with your doctor. This helps if you need to appeal a decision.
- Ask for a referral to a private provider if you’re eligible for public subsidies. Some private clinics accept public funding for specific procedures.
- Consider a private health insurance plan-even a basic one can cover priority access to imaging or specialists.
- Join patient advocacy groups. In New Zealand, groups like Health Advocacy Aotearoa have helped reduce wait times by pushing for policy changes.
Free healthcare gives you a right to care. But it doesn’t guarantee timely, high-quality care. Understanding the trade-offs helps you make smarter choices-for yourself and your family.
Is free healthcare really free?
No. Free healthcare is paid for through taxes. In New Zealand, the average household contributes over $8,000 annually to fund the public system. You don’t pay at the point of service, but you pay upfront through your income and GST taxes.
Why do private healthcare wait times matter if I’m on the public system?
They don’t directly affect you-but they show how resources are distributed. When private clinics have shorter waits, it’s often because they invest in more staff, newer equipment, and faster processes. That’s the same infrastructure the public system lacks. The difference isn’t just money-it’s how efficiently care is delivered.
Can I get private treatment while still using public healthcare?
Yes. Many people in New Zealand use public healthcare for emergencies and basic care, but pay privately for faster scans, specialist visits, or elective surgeries. Some private providers even accept partial public funding if you qualify for subsidies.
Does free healthcare mean worse outcomes?
Not always. For basic care like vaccinations, prenatal visits, and emergency treatment, public systems perform just as well as private ones. But for complex, time-sensitive conditions-like cancer, heart disease, or chronic pain-delays in diagnosis and treatment can lead to worse long-term outcomes.
Are there countries with better free healthcare systems?
Some, like Germany and France, combine universal access with mandatory private insurance, giving people more choice without losing coverage. Others, like Sweden, fund care through taxes but allow private providers to deliver services under public contracts. These models reduce wait times without abandoning universality.
