Disadvantages of Private Healthcare
When discussing private healthcare, a model where individuals pay directly or through private insurance for medical services. Also known as private medical care, it often promises quicker appointments but hides several drawbacks. While many think private healthcare saves time, the reality is often different.
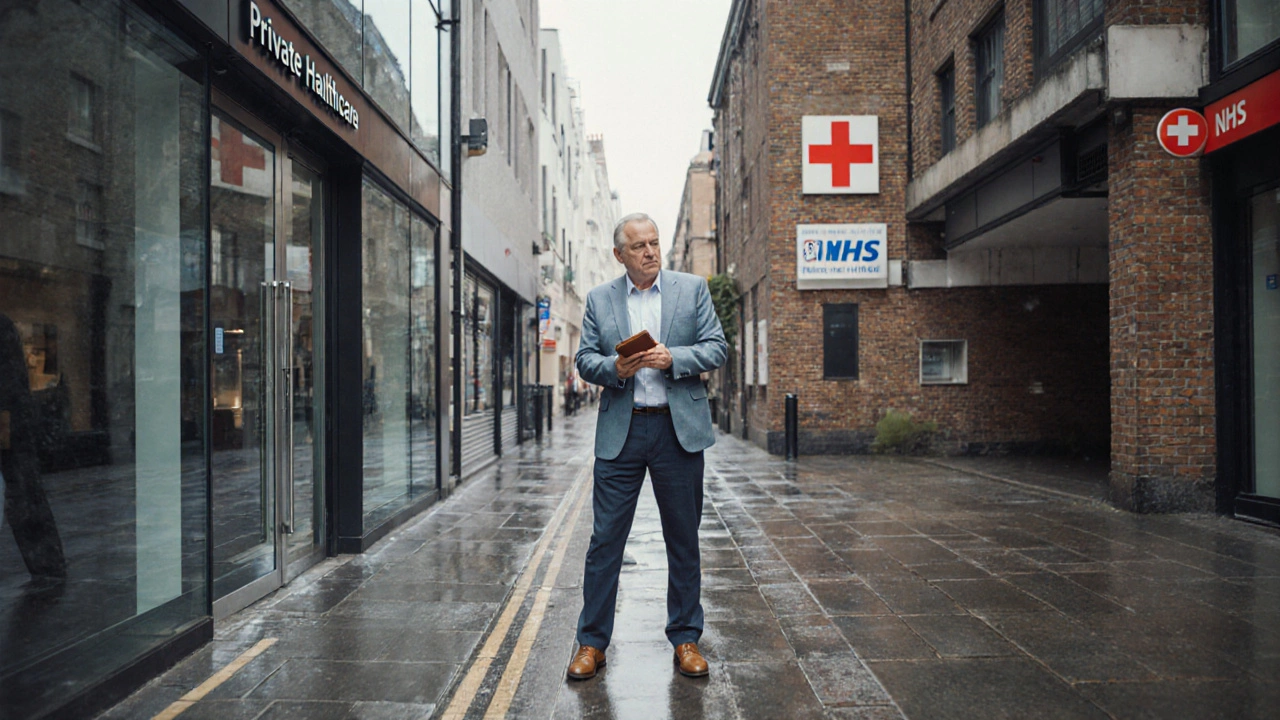
One major contrast is with the NHS, the United Kingdom’s publicly funded health service that offers care based on need rather than ability to pay. The NHS aims to provide universal coverage, which reduces financial barriers for most citizens. However, the existence of the NHS also creates a feedback loop: long waiting lists push some patients toward private options, and those private choices can increase overall system costs.
Speaking of waiting lists, the waiting list, the backlog of patients awaiting treatment in public hospitals is a key driver behind the growth of private providers. When wait times stretch beyond months, people often feel pressured to spend more on private care just to get timely treatment. This dynamic can turn a short‑term decision into a long‑term financial strain.
Financial strain is amplified by health insurance, private policies that cover part or all of medical expenses for individuals. Premiums have risen sharply as insurers negotiate higher fees with private hospitals. Moreover, many policies include high deductibles, co‑pays, or exclusions that leave patients paying out‑of‑pocket for basic procedures. When the cost of insurance climbs, the promised benefit of faster care often disappears.
Key Drawbacks to Watch
First, out‑of‑pocket costs can be staggering. Even a routine surgery that costs a fraction of a public hospital’s fee can balloon to several thousand pounds after adding surgeon fees, facility charges, and post‑operative care. These hidden expenses are rarely discussed up front, leaving patients surprised by the final bill.
Second, the profit motive can influence treatment decisions. Private clinics may prioritize higher‑margin procedures, recommend additional tests, or schedule follow‑ups that aren’t medically necessary. This creates a subtle pressure on patients to consent to more care than they truly need, inflating costs without improving outcomes.
Third, continuity of care often suffers. Because private providers may not share records with the NHS, patients can end up with fragmented medical histories, duplicate tests, or conflicting medication plans. Lack of a unified record makes it harder for doctors to see the big picture.
Fourth, geographic inequality is a real concern. Private hospitals tend to cluster in affluent areas, leaving rural or low‑income regions with limited options. This uneven distribution pushes people in underserved areas to travel long distances, adding travel costs and time to an already expensive equation.
Finally, quality control varies. While many private facilities meet high standards, some operate with less oversight than public hospitals. The drive to cut costs can lead to understaffing, older equipment, or shortcuts in infection control, potentially compromising patient safety.
All these points tie back to the core idea that private healthcare, despite its promise of speed and choice, often brings higher costs, uneven quality, and extra administrative hassle. Understanding these disadvantages helps you make an informed decision about whether the extra expense is worth it for your situation.
Below you’ll find a collection of articles that dig deeper into each of these issues – from cost breakdowns and insurance pitfalls to real‑world stories about waiting lists and quality concerns. Keep reading to see how each disadvantage plays out in practice and what you can do to protect yourself.
Disadvantages of Private Healthcare in the UK - What You Need to Know
Explore the key drawbacks of private healthcare in the UK, including high costs, equity gaps, variable quality, and regulatory challenges, to make an informed decision.