Gender‑Affirming Surgery: What You Need to Know
When exploring gender‑affirming surgery, medical procedures that align a person’s physical characteristics with their gender identity, you quickly run into a mix of medical, legal, and financial questions. The broader field of transgender health, care that supports gender‑diverse people from diagnosis through aftercare provides the backdrop for every decision, from hormone therapy to post‑operative support. In the UK, NHS coverage, public funding for eligible procedures can make the difference between a waiting list of years and a timely operation. Meanwhile, private clinics promise faster slots but come with higher out‑of‑pocket costs and distinct insurance considerations.
Key Factors to Consider
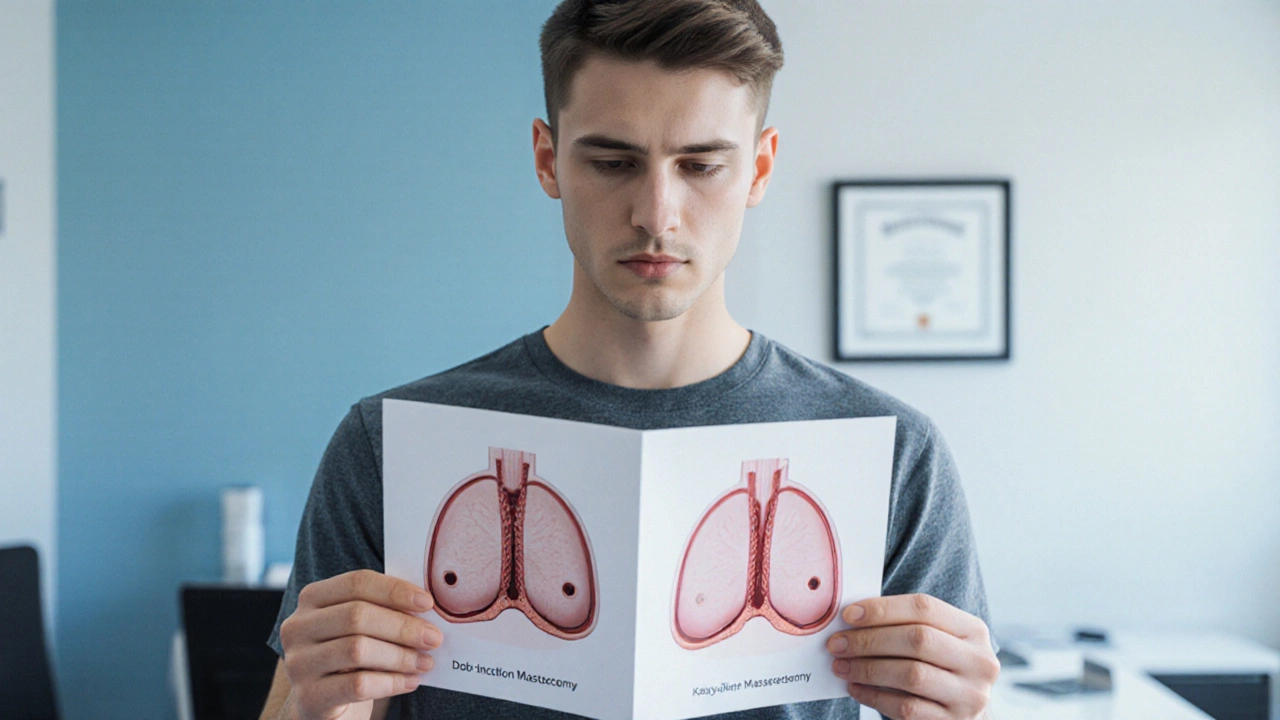
First, understand that gender‑affirming surgery includes a range of procedures—vaginoplasty, phalloplasty, chest reconstruction, and facial feminization, among others. Each procedure carries its own risk profile, recovery timeline, and skill requirements for the surgeon. Psychological assessment is another mandatory step; guidelines from bodies like WPATH (World Professional Association for Transgender Health) state that a thorough mental health evaluation must precede any operation. This assessment helps match patients with the right surgical plan and ensures postoperative wellbeing.
Cost is a major driver of choice. A recent US‑UK cost comparison showed that US patients often pay 2‑3 times more for comparable surgeries, even after insurance rebates. In the UK, NHS funding applies only when certain criteria are met, such as documented gender dysphoria and a minimum period of hormone therapy. Private insurance plans in the US may cover part of the bill, but they frequently require pre‑authorization and limit the number of covered procedures. Understanding these financial pathways can prevent surprise bills later.
Safety standards vary by setting. The UK’s NHS mandates strict surgeon credentialing and audit processes, which can lower complication rates. Private clinics in high‑volume centers often adopt similar standards but may prioritize speed over comprehensive follow‑up. When evaluating a surgeon, look for board certification, specific experience with the desired procedure, and published outcome data. Independent safety checklists—like those used for cosmetic surgery—are useful tools to compare clinics.
Post‑operative care is just as critical as the operation itself. Recovery can involve wound care, catheter management, and physical therapy, especially for phalloplasty or vaginoplasty. Access to a multidisciplinary team—including surgeons, endocrinologists, mental‑health professionals, and physiotherapists—greatly improves long‑term satisfaction. In the NHS, these services are often integrated under a single care pathway, while private patients may need to coordinate multiple providers.
Insurance and funding also shape the timeline. While NHS patients may face waiting periods of up to several years, private patients can schedule surgery within months—but must budget for the full cost, which can range from £10,000 to £80,000 depending on the procedure and hospital. Some charities and grants exist to offset these expenses, especially for younger patients. Checking eligibility early can smooth the financial planning process.
Legal and administrative steps shouldn’t be overlooked. In the UK, patients must navigate the NHS referral system, which includes referrals from GPs and specialist gender clinics. Documentation of hormone therapy, mental‑health assessments, and a clear surgical plan are all part of the application. In the US, consent forms, insurance pre‑authorizations, and sometimes legal name‑change paperwork are required before the surgeon can proceed.
Finally, keep an eye on emerging trends. Tele‑health consultations for pre‑operative assessment are growing, offering easier access to specialist advice, especially for patients living far from major centers. At the same time, research into newer techniques—such as minimally invasive vaginoplasty or advanced flap methods for phalloplasty—continues to improve outcomes and reduce recovery time.
Below you’ll find a curated set of articles that dive deeper into each of these areas: cost comparisons, safety rankings, NHS versus private pathways, and practical tips for managing post‑surgical recovery. Use them to build a clear, personalized plan that balances your health goals with realistic expectations.
How to Afford Top Surgery: Cost Breakdown & Funding Options
A practical guide breaking down top surgery costs, key price drivers, and proven ways to fund the procedure, from insurance to grants and budgeting tips.